Advanced Monitoring Parameters: GEDI
Preload - Global End-Diastolic Volume Index (GEDI)
The preload is, along with afterload and contractility, one of the determinants of stroke volume and therefore cardiac output. Theoretically, it can be best described as the initial stretching of a single muscle cell of the heart prior to contraction, which means at the end of diastole. As this cannot be measured in vivo, other measurements have therefore to be substituted as estimates. In the clinical setting, preload is referred to as the end-diastolic pressure or (more precisely) end-diastolic volume. A higher end-diastolic volume implies higher preload.[1]
In the clinical setting, preload is referred to as the end-diastolic pressure or (more precisely) end-diastolic volume
A higher central venous pressure (CVP) and / or a higher pulmonary capillary wedge pressure (PCWP) is still often regarded as an indicator of higher preload (CVP for the right heart, PCWP for the left heart). This is mainly due to the limitation that pressure cannot be directly transferred into volume. So any volumetric parameter assessing the filling of the ventricle at the end of diastole reflects the actual preload more precisely.
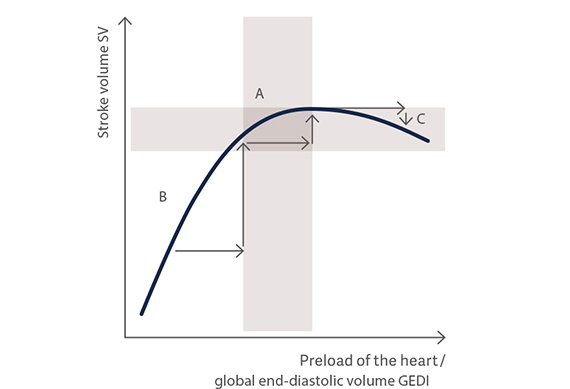
Frank-Starling Mechanism
The Frank-Starling law states that the greater the volume of blood entering the ventricle during diastole (end-diastolic volume), the greater the volume of blood ejected during systolic contraction (stroke volume) and vice-versa. This is an adaptive mechanism of the organism to compensate for slight changes in the ventricular filling.
The power of the heart muscle depends on its initial load before the start of contraction
However, it can also be used to increase stroke volume by volume administration for therapeutic reasons. The force that any single cardiac muscle fibre generates is proportional to the initial sarcomere length (known as preload), and the stretch on the individual fibres is related to the end-diastolic volume of the ventricles.
An increase in preload will, to a certain extent, lead to an increase in stroke volume (SV), based on optimal myocardial muscle fibre pre-stretching. Up to a certain limit, the more the sarcomeres of the muscle cells are stretched the greater the contraction. On the other hand, contractility may decrease in conditions of volume overload.
Schematic Frank-Starling curve for verification of the preload status
A = Optimal preload, B = Volume responsive, C = Volume overload