个性化通气方案
因为每个患者本就不同

每个病人都面临着特殊的挑战。不论是体重 300 克新生儿还是成人,不论是患有急性呼吸衰竭还是慢性肺部疾病的人,他们的需求和复杂性都是不同的。这就是为什么我们致力于创新个性化的通气解决方案,以帮助保护肺部和其他器官,加速撤机以获得更好的结果。

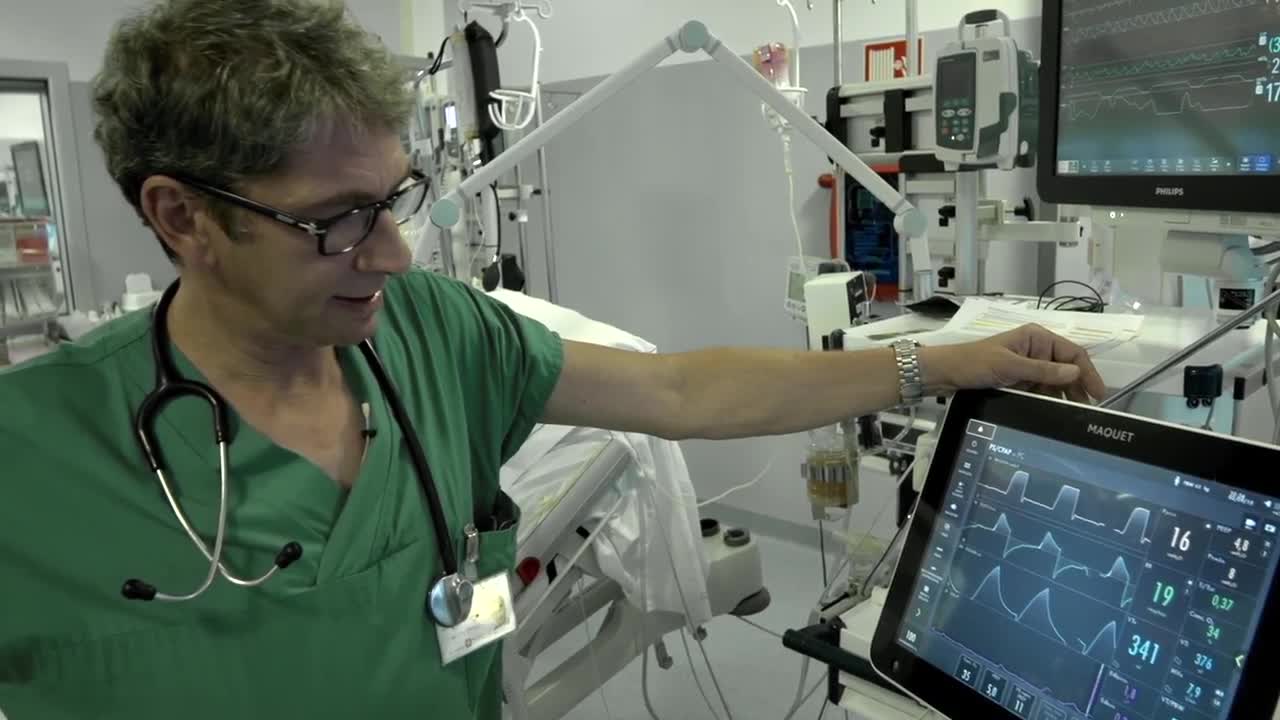
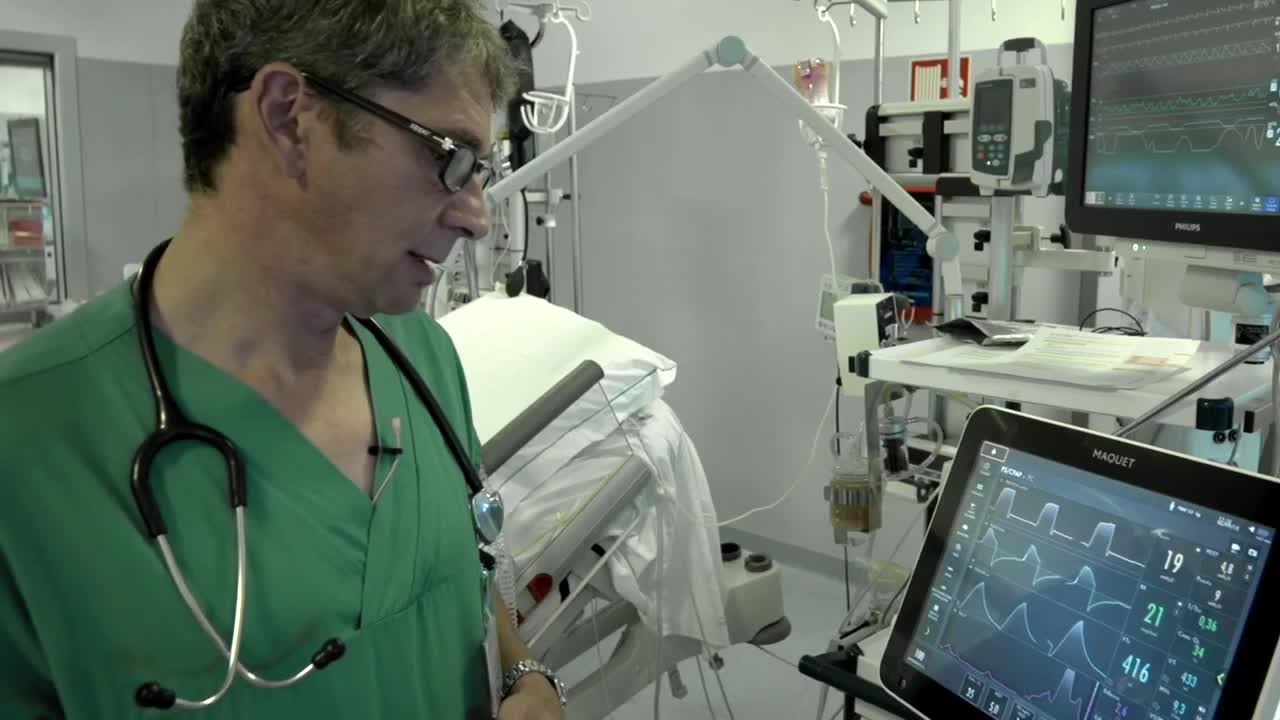
提供定制化的肺保护 – 使用工具来定制治疗方案
为了个性化病人与呼吸机的交互,并防止呼吸机引起的肺损伤,我们提供了一个强大的工具包来提供定制的肺保护。所有的设计都是在医院的行为准则的基础上为您提供支持服务。

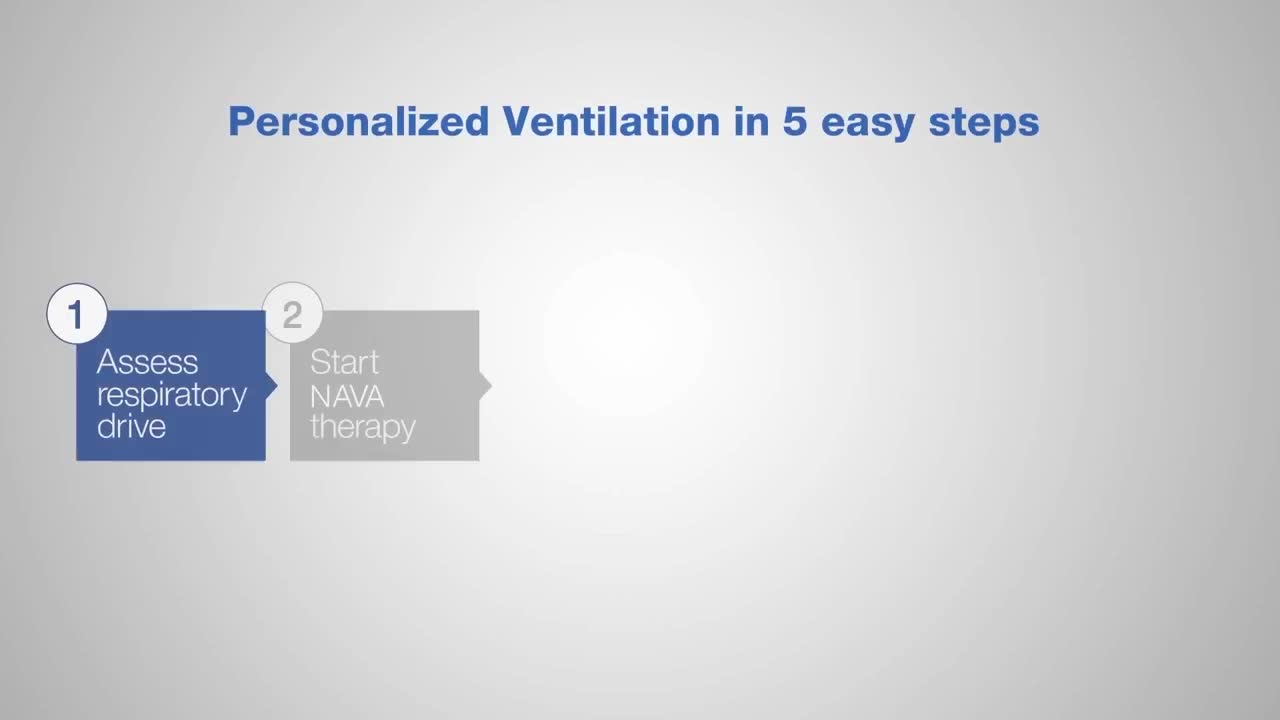
提供定制化的撤机 – 使用工具来帮助患者轻松脱离呼吸支持
想要稳定病人,减少镇静和使病人脱离呼吸机的过程更加轻松那么可能需要个性化的撤机功能。我们的 Servo 呼吸机提供了许多工具,可以在撤机过程中帮助到临床医生和患者。比如我们的 NAVA 通气模式,无创 NAVA 和高流量氧疗。

找到定制化的解决方案以满足您的要求
有了 Servo 系列,您可以根据您病人的特点,设置和医院的要求,选择合适的 Servo 呼吸机。它灵活和易于使用,你可以进一步通过个性化的工具,帮助患者减少并发症和早期撤机,无论是有创还是无创通气,从 ICU 到中间护理,所有类别的患者都可以适用。

Servo 呼吸机故事
这是一个革新的故事。它将改变我们对重症监护通气的看法,提出了个性化通气的概念。
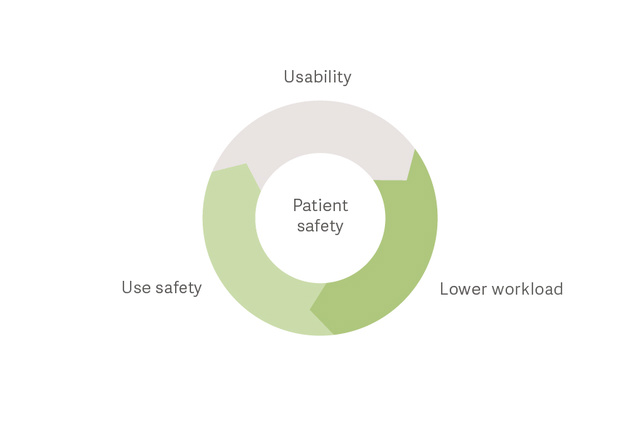
增强患者安全性
提供适宜的通气,尽早撤机
研究表明,许多 ICU 患者会产生呼吸困难。这些患者可能面临着多次通气挑战 [5],消耗了大量呼吸功。[6] 向下滚动,了解如何帮助应对这些挑战。

挑战: 避免对呼吸衰竭患者插管
无创呼吸支持可减少插管的需要和由此产生的并发症,如呼吸机相关肺炎(VAP)、[7] 过度镇静、[8] 谵妄、 [9] 和 ICU 获得性虚弱。[10] 无创支持允许患者保持活动,这是目前许多 ICU 采用的策略。Servo-u提 供多种选择,以支持您的患者与无创性治疗。
挑战: 在控制通气过程中预防呼吸机引起的肺损伤
有时有必要完全控制病人的呼吸。气压伤,容积伤等都是潜在的后果。但它们的发生率可以降低。[11] [12] [13] 通过视频了解更多信息。

早期保护性机械通气是 ARDS 预后的关键
Lungsafe 研究表明,保护性通气并没有得到一致的应用,这反映了需要更些容易获得且有效的床旁工具来识别肺部危险。这项重要的研究得出结论,ARDS 未被充分认识,治疗不足,仍然与高死亡率相关。
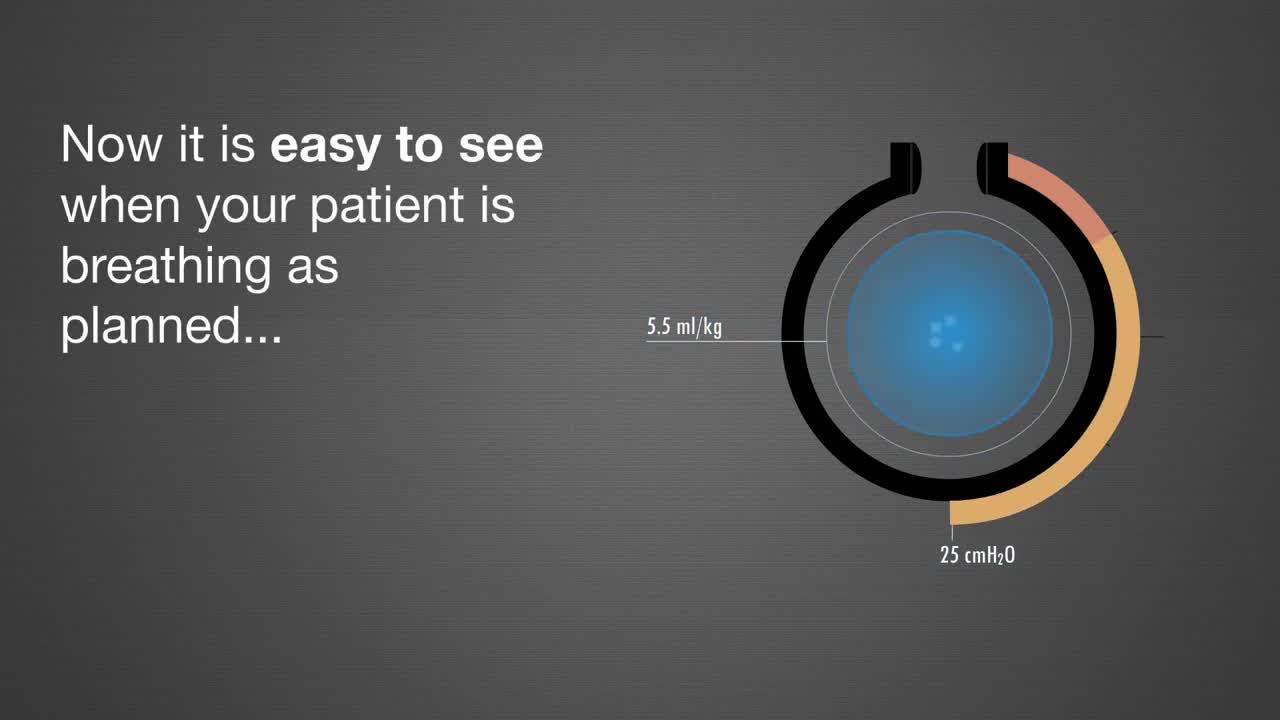
挑战: 预防辅助通气时呼吸机引起的肺损伤
研究表明,神经调节呼吸辅助 (NAVA®) 可大大的改善人机同步性,促进气体交换,进行肺保护性通气。[14] [15] 使用NAVA时,当肺部过度膨胀,呼吸中枢反射会立即限制潮气量改变。这种呼吸模式可使患者选择自己所需要的潮气量,降低VILI的发生。[16] [17]
挑战 : 避免呼吸机引起的隔肌功能障碍 (VIDD)
膈肌厚度在机械通气 48 小时后可降低 21%。[18] 识别膈肌可能很复杂,[19] 但不可或缺。监测Edi信号可以反应患者的膈肌活动,而 NAVA个性化的通气可以提高膈肌效率,减少过度辅助。[20] [21] 请观看视频了解更多关于 Edi 信息。
挑战 : 避免通气过程中患者与呼吸机的不同步
人机不同步患者治疗效果较差,通气时间较长;[22] [23] [24] [25] 人机不同步患者占 ICU 所有镇静使用的 42%,[26] 监测膈肌活动 (Edi) 使检测不同步更方便,可以根据患者需要调整呼吸机的设置。[27] 观看视频 Edi 是如何工作的。

挑战 : 防止延迟撤机
最近的一项研究显示,29% 的患者由于膈肌功能障碍而出现撤机失败致使机械通气时间延长至 16 天。[18] 但是拥有NAVA呼吸机,减少镇静剂的使用,运动膈肌使患者更舒适,这可能有助于促进更早撤机。[2] [3] [4] 此外,监测膈肌活动 (Edi) 可以帮助评估撤机准备情况,并可在撤机后监测恢复过程中呼吸中枢做功情况。[27]
让您的呼吸机适应各种条件
确保投资回报,令您收益稳定无压力

成本效益
SERVO 呼吸机易于学习和使用,需要清洗的部件少,维护方便,缩短培训时间增加培训质量和工作人员的效率。
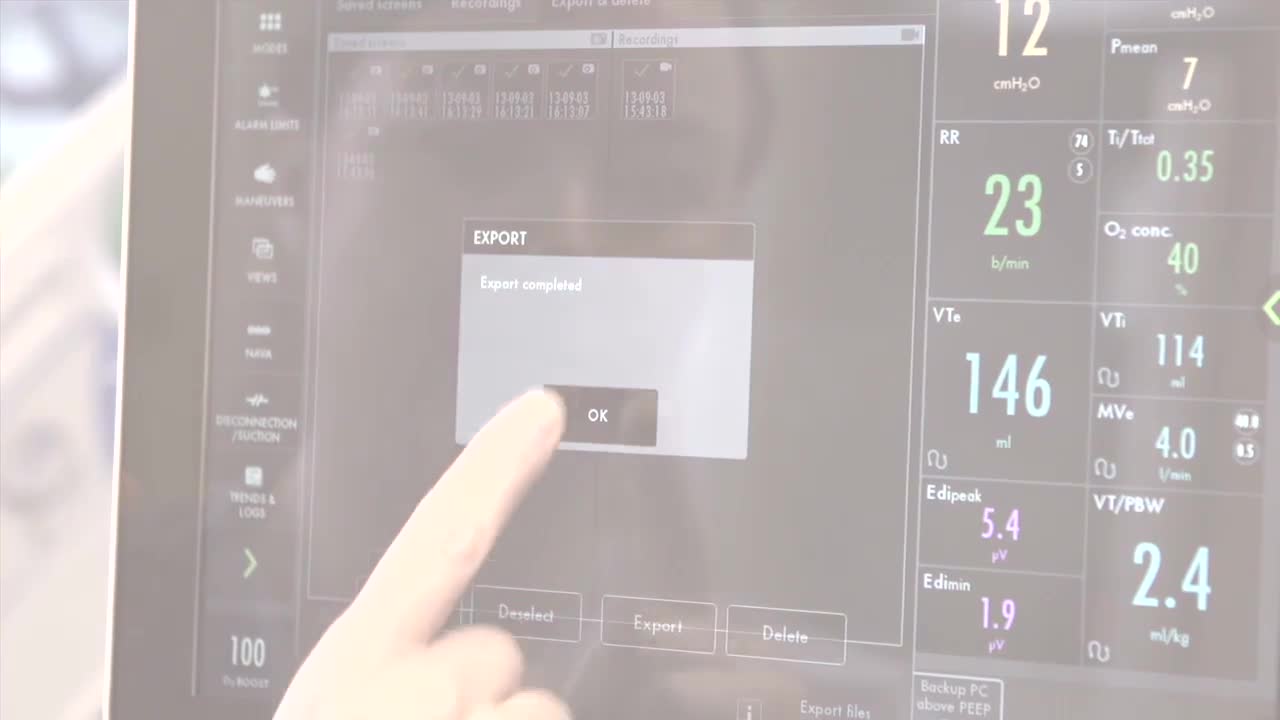
连接环境
SERVO 呼吸机可连接到多个PDMS系统和患者监视器。[1] An HL7 变换器使系统符合IHE 技术指标。
智能机器管理
SERVO 呼吸机相似的外观,可互换的插件模块,超高灵敏度,更多的移动解决方案,使其更加便于管理易于使用使用。
可扩展的服务程序
远程服务可以连接任何医院的计算机查看和访问设备的信息。一系列高品质的耗材和部件将确保 SERVO 呼吸机的先进性。