Using the electrical activity of the diaphragm (Edi) to evaluate ICU patients’ need for respiratory support is a valuable and often superior complement to standard monitoring parameter, according to senior respiratory consultant Sten Borgström.
In many cases, it can cut evaluation times significantly. Getinge sat down with the Swedish pioneer of using Edi signals for respiratory monitoring and asked him to describe his experiences.
Understanding the patients' breathing
Monitoring the brain’s neurological impulses to the diaphragm (Edi) transforms the care that can be provided to patients on a ventilator. Interpreting the Edi signal on a routine basis enables doctors to understand the patient’s true condition and desired breathing pattern. According to Dr Sten Borgström, MD, DEAA, using Edi can speed up patient care and lead to shorter time spent on a ventilator.
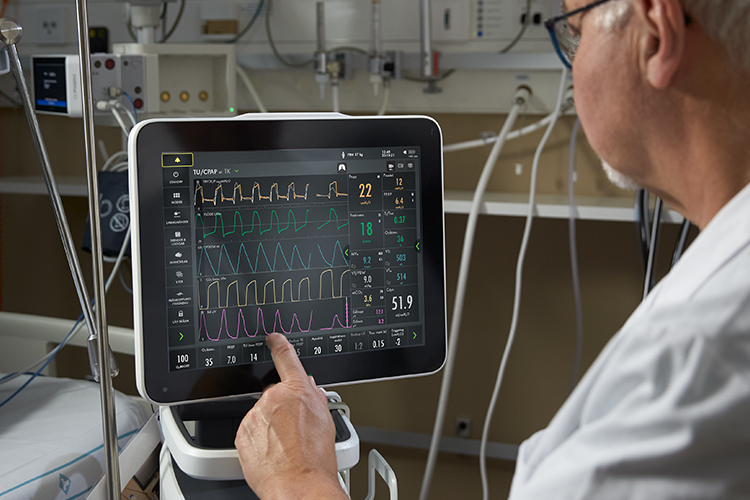
“In the past it would take maybe 30 to 35 minutes to work out why a patient was struggling to breathe spontaneously. With the Edi signal, this information is available directly,” he says. Edi monitoring requires the insertion of an Edi catheter, a nasogastric tube with 10 electrodes that receives the Edi signal and also functions as a feeding tube. The catheter connects to the ventilator and the Edi signal is displayed on the ventilator's screen, providing continuous information about the magnitude and timing of the patient's drive and breathing effort.
Dr Borgström began using Edi readings in 2008 while working as senior consultant and medical director at Kalmar Hospital in southern Sweden. “In the beginning I used Edi simply for the purpose of getting the NAVA ventilation mode to work effectively. The Edi signal was nothing more than an instrument to find the right NAVA level,” he says.
“As time went by I started thinking about what the Edi signal actually is and what influences it, and I began to realise how it can help us in so many different areas. Pre-intubation, weaning and post-extubation care are just a few. For us, Edi went from being a single-purpose tool to an application covering a very wide spectrum of medical knowledge.”
For me it would be a major step backwards if I didn’t have access to an Edi signal
Benefits throughout the care process
The advantages begin at the start of the care process. Physicians use a wide range of respiratory parameters to monitor and assess the patient’s breathing. When evaluating new patients, Dr Borgström and his colleagues have found that Edi readings are not only a valuable complement to standard parameters, but are also often superior – and in most cases faster and more effective to use.
“It’s possible to use Edi readings to decide if you need to intubate a patient from the outset or if he or she has fundamentally healthy lungs, making the intubation option less urgent and allowing the medical team to proceed instead with non-invasive ventilation using NIV NAVA,” Dr Borgström explains.
He sketches a scenario in which the patient’s respiratory rate has risen from 18 to 28 and their Edi signal and amplitude have also increased sharply. “I now have two criteria on which to decide whether to intubate or not. In fact, the Edi signal often reacts much faster than respiratory rate or desaturation.”
"Edi provides critical advance warning”
Dr Borgström believes the body senses an atelectic tissue trend early on – long before physicians can observe it through reduced oxygen saturation. In this context, the Edi signal provides critical advance warning to him and his team when assessing the patient’s underlying condition.
“I can insert an Edi catheter and clearly see if the Edi signal amplitude is increasing. This tells me that the patient’s condition is deteriorating and that we must intubate. It’s a piece of the puzzle that can play an important role in creating an overall picture and determining whether we should intubate immediately, wait a while, or perhaps use non-invasive NAVA ventilation,” he says.
Conversely, Edi can also be used as a diagnostic tool to eliminate as well as confirm the need for ventilation. Dr Borgström recalls a patient with a neck injury initially believed to be a fracture including the spinal cord.
“We inserted an Edi catheter and discovered perfect Edi signal, which told us that it wasn’t a cross-sectional lesion at all but a spinal cord injury with heavy bruising,” he says. “So we went from thinking that we had a patient who would be unable to breathe for the rest of his life and might not even survive intensive care, to a patient with a fully functional breathing pathway from the brain stem to the diaphragm. That patient was able to breathe unassisted and recovered, albeit with some paralysis.”
Revealing the true state of a patient’s lungs
As a patient undergoes treatment, the Edi signal can be an important aid in determining how the recovery is progressing and assessing the underlying state of the patient’s lungs. According to Dr Borgström, the signal can reveal if a lung is fundamentally healthy, moderately sick and obstructive, or very sick and obstructive.
“Edi readings enable us to talk in terms of physiology and pathophysiology instead of a mechanical pump that pumps air in and out of the tissue that we call the lungs. We can clearly see how the Edi signal develops over time in a chronically ill patient connected to NAVA and how Edi amplitude gradually reduces as the lungs recover – and how this process greatly depends on the lungs’ underlying condition,” Dr Borgström says.
He adds: “It’s a very large piece of the jigsaw puzzle for me, and I believe that using [the Edi signal] protects the patient from lung injury.” This is because Edi data can reveal the presence of atelectasis or fluid in the lung.
Minimising the patient’s time on the ventilator
Equally, Edi readings can play a valuable role in the often-complex process of weaning patients off a ventilator. Edi data can be used to measure the patient’s ability to breathe spontaneously, allowing the clinical team to ascertain if the patient’s condition indicates that weaning is premature.[1] Other values used in the weaning phase, including blood gas and saturation, take longer to measure and interpret.
Dr Borgström’s experience, It is also possible to use Edi readings to avoid reintubation, thus averting the need to go back to invasive ventilation, which may otherwise prolong treatment. “If you see a sharp increase in Edi amplitude you will know much earlier that reintubation needs to be considered,” says Dr Borgström. “In some cases the information may even enable you to avoid reintubation by putting the patient into non-invasive ventilation with or without NIV NAVA before reaching the point where reintubation would have been necessary.”
So we went from thinking that we had a patient who would be unable to breathe for the rest of his life and might not even survive intensive care, to a patient with a fully functional breathing pathway from the brain stem to the diaphragm. That patient was able to breathe unassisted and recovered, albeit with some paralysis.
There’s no going back
Dr Borgström likens an absence of Edi data to wearing a pair of glasses with a 10-year-old prescription and cheap lenses. “For me it would be a major step backwards if I didn’t have access to an Edi signal,” he says. “I couldn’t give the patient the best possible care. Not using NAVA and Edi readings dramatically raises the risk of harmful patient-ventilator asynchrony.”
Patient-ventilator asynchrony is a mismatch between the patient and ventilator, regarding time, flow, volume, or pressure demands of the patient respiratory system. It is a common phenomenon.[1],[3] Asynchrony incidence rates range from 10 % to 85 % and may be caused by factors related to the patient, to the ventilator, or both.[2]
The most common types are:
- Triggering, such as ineffective effort, auto-triggering, and double triggering
- Asynchrony related to premature or delayed cycling
- Asynchrony arising from insufficient or excessive flow
Each type is difficult to detect by visual inspection of volume, flow, and pressure waveforms on the mechanical ventilator display.[4] Asynchrony has been associated with unwanted outcomes such as discomfort, dyspnea, deterioration in pulmonary gas exchange, increased breathing effort, diaphragmatic injury, sleep impairment, and increased use of sedation or neuromuscular blockade. It has also been linked to increases in mechanical ventilation length, weaning time and mortality.[5]
The Edi signal helps the physician to tailor sedation levels better to patient need and to provide just the right level of medication to calm the patient – without oversedation, removal of respiratory drive and risking prolonged care.[6] Greater accuracy in sedative dosing is also beneficial for the Edi readings themselves. This is because sedatives and analgesics can affect the Edi signal, respiratory drive and other vital parameters.
Using the Edi signal

- The Edi overlay helps you identify patient-ventilator asynchronies. For example, if you look closer at the first breath, it shows a late cycle off (yellow curve) where the patient receives a full breath when wanting to exhale (grey cuve).
- The Edi waveform and trend window can be used to monitor the level of support needed.
