What is low-flow anesthesia?
In low-flow anesthesia, a rebreathing system uses a fresh gas flow (FGF) that is less than the minute ventilation of the patient. This approach allows a significant portion of the exhaled gases, except carbon dioxide (which is absorbed), to be rebreathed by the patient.
Low flow is generally characterized by a FGF of less than 1.0 L/min. There are various gradations within the FGF spectrum, such as low flow, minimal flow or metabolic flow, which refer to the further reduction of FGF. For Dr. Jan Hendrickx, Anesthesiologist at OLV Hospital in Aalst, Belgium, these historical terms refer to just three points of the entire FGF spectrum of 1, 0.5, and 0.2 L/min, respectively: “Although these terms are widely used, it's more precise to reference the specific FGF in use. A term gaining traction, lower flow anesthesia, emphasizes adapting to a FGF below one's current usage. Rather than adhering to a strict FGF definition, it's about evolving one's practice to the lowest FGF level one is comfortable working with. Such target-controlled low flow makes the traditional distinctions of flow somewhat arbitrary.”
Unpacking multifaceted benefits
Low-flow anesthesia emits less gas into the atmosphere, and improves the gas composition of the inhaled air:
- Environmental benefits: Decreased pollution and waste
All anesthetic gases act as greenhouse gases and ultimately release into the atmosphere. Some halogenated anesthetics have a global warming potential up to 7,020 times that of CO2[1], with desflurane being the most impactful. Low-flow anesthesia limits the release of these agents into the environment. Dr. Hendrickx highlights the reduced wastage of inhaled anesthetics as a significant advantage of low-flow anesthesia, stating, “The circular breathing system employed with low flow essentially acts as a recycling system." In line with this, he recommends minimizing the use of the most harmful vapors and gases, such as desflurane, to minimize the environmental impact from inhalation anesthetics in hospitals. - Pulmonary benefits: Preserving warmth and humidity
”An added advantage is the enhanced heating and humidity of the typically cold and dry gases entering the circle breathing system from the operating room wall outlets. The lower the FGF, the more CO2 is processed through the absorber, resulting in increased production of H2O and heat.“ This optimization boosts mucociliary clearance, stabilizes body temperature, diminishes water loss, and heightens both patient comfort and safety[2]. - Economic benefits: Reduced costs
The cost of anesthetic agents can constitute a significant portion of the overall expenditure for anesthesia machines, depending on the FGF. Decreasing agent consumption yields positive economic implications for healthcare institutions. - Educational benefits: Deeper understanding of pharmacokinetics
Paying closer attention and being more observant contributes to a deeper grasp of pharmacokinetics, marking a vital advantage of low-flow anesthesia. - Safety benefits for OR staff: Minimized leaks
By reducing surplus gas released into the environment, the concentration of anesthetic gas in the operating room drops significantly. This diminishes occupational hazards for OR personnel.
Remarkably, the benefits of using a re-breathing system during anesthesia have been known since 1924, underscoring its enduring value for almost a century[3].
Challenges in manual low-flow anesthesia
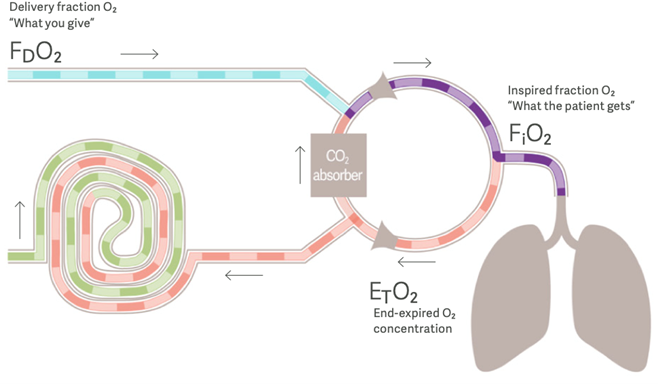
For a safe manual control during delivery, it is essential to understand the differences between FGF, minute ventilation, the delivered concentration, and the inspired concentration, as well as to use a gas analyzer. Failing to adhere to these principles can cause anesthetic overdosing or underdosing, leading to hypotension and patient awareness, as well as insufficient O2 dosing, producing inspired hypoxic mixtures. Dr. Hendrickx points out that this is why manually controlled low flow is often perceived as challenging or risky in practice:
- Difficult: Lowering fresh gas flows increases the difference between the preset concentration delivered and the one actually inspired by the patient. The lower the FGF, the more pronounced this difference becomes. This can give a sense of lost control, as what's "delivered" doesn't equate to "what the patient receives".
- Unsafe: One of the most significant risks of using low-flow anesthesia is the formation of hypoxic mixtures. Reducing fresh gas flow in a rebreathing circle system can dilute the inspired O2 during rebreathing (fig. 1). As a result, the inspired oxygen may fall below the delivered fraction. If this discrepancy isn't promptly recognized and addressed, hypoxic mixtures can emerge.
- Cumbersome: “Lowering the FGF in inhaled anesthetics can cause discrepancies between the delivered and inspired concentrations, induce a slower wash-in, necessitate more frequent vaporizer adjustments, make it more difficult to predict settings for individual patients, and may cause oscillations in target end-expired agent concentration. This effect intensifies as FGF decreases”, says Dr. Hendrickx. Continual manual adjustments are required, which might elevate the risk of improper anesthetic gas levels and insufficient anesthesia depth. "Traditional teachings tend to overemphasize mathematics, but low flow is straightforward. No advanced math is required when applying these principles to both inhaled agents and O2."
“Target-controlled low-flow anesthesia in a closed-loop system solves all the above issues,” says Dr. Hendrickx. "Instead of manually controlling flow meters and vaporizers, clinicians now instruct the anesthesia workstation equipped with an Automatic Gas Control (AGC) to maintain specific end-expired anesthetic and O₂ concentrations. The workstation automatically adjusts flow meter and vaporizer settings to reach those target concentrations, helping clinicians to do a great job in minimizing FGF and thus waste[4].”
AGC facilitates the control of oxygen delivery through a single FIO₂ target setting. This setting takes precedence and remains unaffected by the selection of anesthetic agent speed, thereby reducing the risk of hypoxia. It enables the adaptation of agent administration to the patient’s status or surgical incision time and minimizes the risk of under- or overdosing. A speed control and real-time prediction tool enables clinicians to determine the time to end-tidal target, enhancing the efficiency of gas delivery. The positive impacts of AGC are well-supported by both evidence and expert consensus[4],[5].
AGC: A smart investment in sustainability
AGC technology allows for a safe and significant reduction of anesthetic waste, slashing it by up to 58%[5]. "Patient safety is priceless, and environmental protection is crucial. While lower flows cut down on inhaled agent consumption, they also increase CO₂ absorber usage, but all my analyses so far suggest that the combined effect is a decrease in cost and pollution," says Dr. Hendrickx. Tailored models exist to compute these for specific scenarios.
Getinge's Flow anesthesia machines offer the benefits of low flow anesthesia without its drawbacks. Equipped with AGC, Volume Reflector technology, and a vaporizer with fuel injector technology, these machines empower physicians to safely apply minimal-flow anesthesia, reducing anesthesia gas emissions, and minimize costs[4]. In the event that oxygen levels fall below 21%, without clinician intervention, the O₂Guard - the only commercially available active inspired hypoxic guard, steps in to prevent the delivery of hypoxic mixtures, helping to minimize the risk of hypoxia.[6],[7].
Low-flow anesthesia offers a range of benefits, spanning from environmental to economic aspects. However, its challenges have often deterred practitioners. Now, innovative automated systems are transforming this practice, empowering clinicians to leverage its advantages and navigate its complexities seamlessly.
