Reduce the burden of a global health crisis
Everyone is at risk of developing sepsis. Globally, up to 50 million people are affected by sepsis, every year. Every 2.8 seconds, one patient dies from sepsis and associated complications. Often, it can be prevented by vaccination, clean water and hygiene, safe childbirth, and preventing hospital-acquired infections (HAIs). However, sepsis is often underdiagnosed, especially at an early stage where treatments are more successful. [1]
Sepsis is a medical emergency with high mortality rates. Sepsis survivors often suffer long-term disabilities. One out of four sepsis patients does not survive hospitalization. [2], [3]
Sepsis is defined as a dysregulated immune response to an infection that injures the body's tissues and organs. As a life-threatening organ dysfunction, sepsis can lead to shock and multi-organ failure. If not recognized early and treated promptly, sepsis often leads to death. Sepsis is the most common way to die from an infectious disease worldwide, including viruses such as SARS-CoV-2. Hospital-acquired sepsis accounts for more than 40% of mortality rates and is still one of the most common complications in Intensive Care Units. [4], [5], [6]
|
60 - 80% of ICU Patients with sepsis were infected inside the hospital [7] |
100% higher probability to die in the next 5 years [8] |
76.000€ average cost per septic patient in Germany [9] |
What causes sepsis?
- The infection is most commonly caused by infections by bacteria, fungi, viruses, or parasites.
- The primary sources of infections resulting in sepsis are the lungs, abdomen, urinary tract, or skin.
- 50 % of all sepsis cases start as an infection in the lungs.
- No definitive source is found in 35 % to 50 % of cases.
- Endotoxins initiate a pathophysiological cascade.
- Dysregulation of the proinflammatory response of cytokines, which promotes tissue-damaging inflammation.
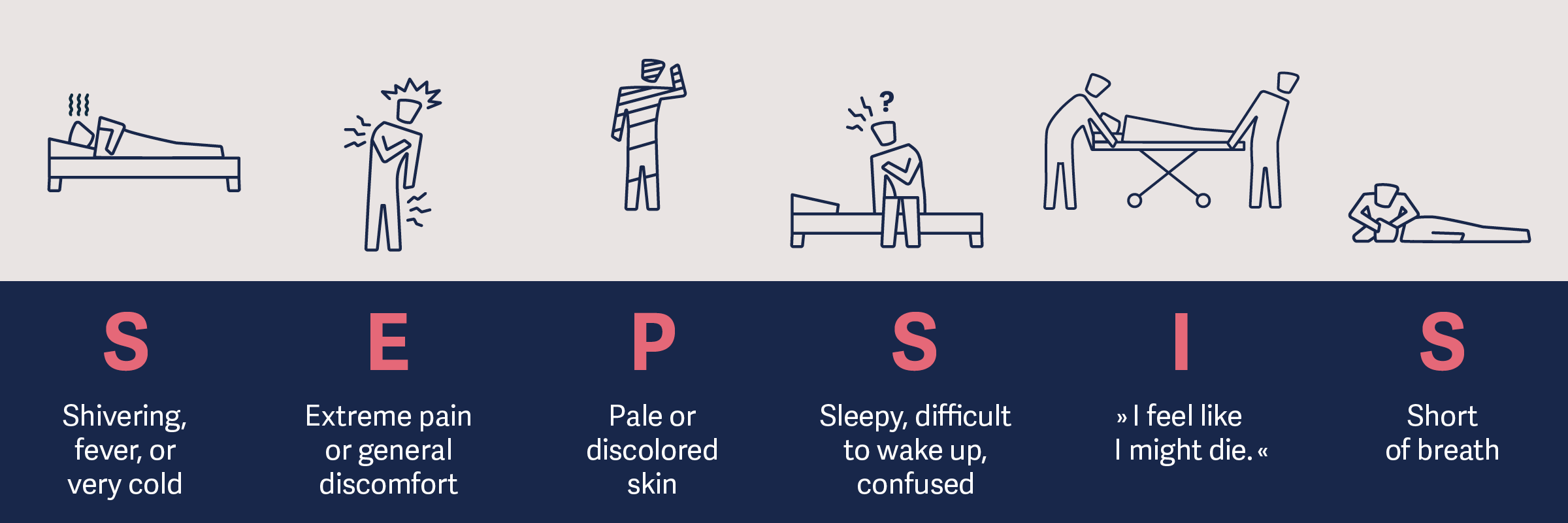
Sepsis symptoms
Sepsis and SARS-CoV-2
"...COVID-19 does indeed cause sepsis."
Today, it's known that COVID-19 can cause severe pneumonia, other organs can be affected by SARS-CoV-2, too. Multi-organ injury, which is typical for sepsis, occurs in 2-5 % of COVID-19 patients, after approximately 8-10 days. Sepsis and its complications are reasons for high mortality amongst COVID-19 patients. Therefore, knowing and recognizing early signs of sepsis is crucial for the initiation of treatment. Timely intervention after diagnosis can save lives and prevent harm to vital organ functions. [10]
Hemodynamic sepsis management
Hemodynamic management is a key therapeutic aspect in treating patients with sepsis or septic shock. [10]
The hemodynamic management of patients with sepsis and septic shock is an important cornerstone for treatment and resuscitation. Delayed or inadequate hemodynamic management can have serious outcomes. Hypoperfusion, tissue hypoxia, edema, and fluid overload, may lead to multiple organ failures. [11]
Hemodynamic stabilization is crucial after a sepsis diagnosis. Deliver immediate fluid resuscitation while obtaining other important laboratory results like lactate levels, blood cultures, and antibiotics is of great importance. [12], [13]. Also, hemodynamic monitoring can help identify the type of sepsis and supports drug management.
The goal of advanced monitoring and managing hemodynamic parameters in sepsis patients is to optimize and restore the balance between oxygen demand and supply at the tissue level. A goal-oriented therapy approach should be followed, ensuring adequate perfusion and the balance of oxygen levels, with a continuous mean arterial pressure above 65 mmHg. [11]
How to use PiCCO for sepsis therapy
PiCCO provides and monitors a number of important parameters including continuous cardiac output at the bedside which can have an impact on clinical decisions. These parameters help identify adequate fluid resuscitation, without the risk of fluid overload. PiCCO monitoring also optimizes the administration of catecholamines and vasoactive agents.
Hemodynamic sepsis management within first 24 hours
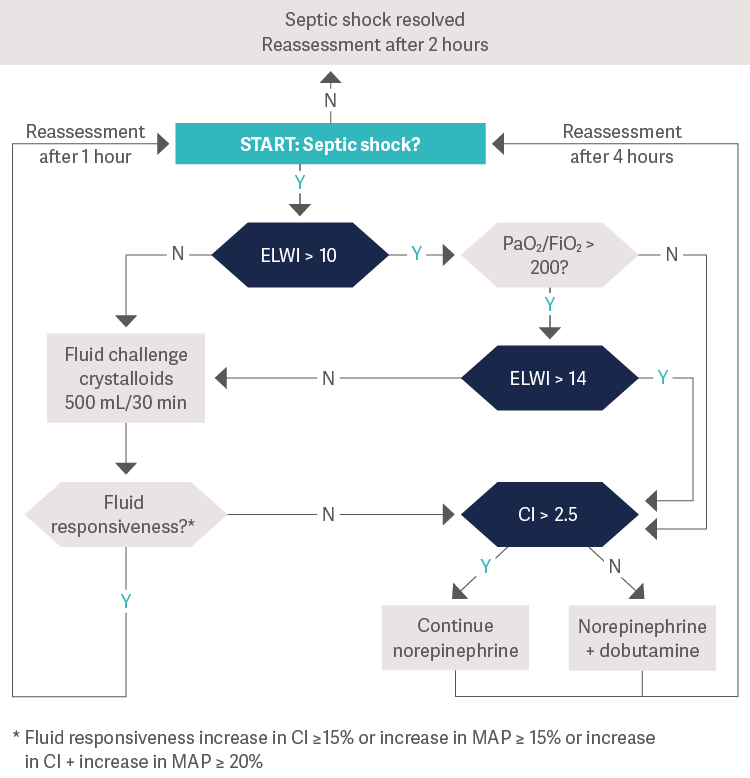
[11], Values measured in: CI = L/min/m2 · GEDI = mL/m2 · ELWI = mL/kg · MAP = mmHg
Hemodynamic sepsis management after first 24 hours
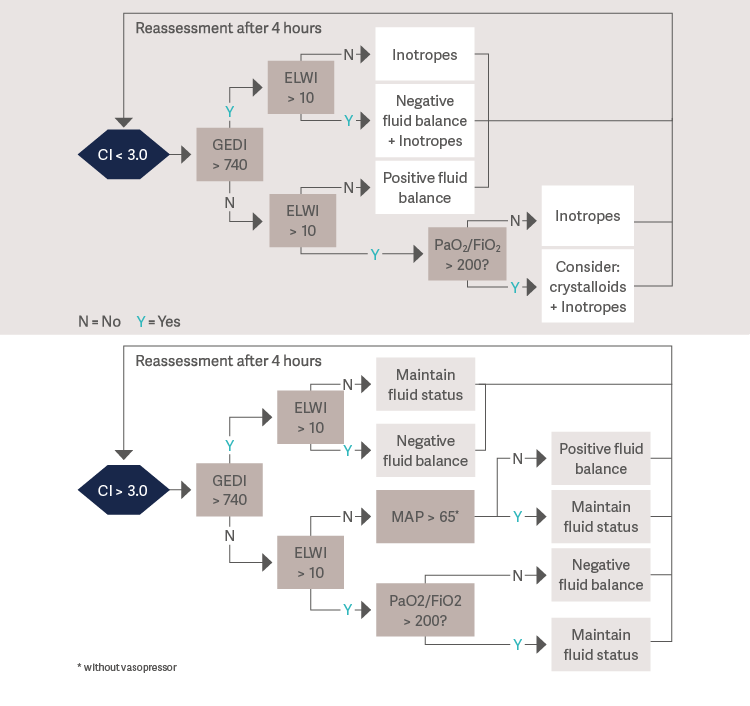
[11], Values measured in: CI = L/min/m2 · GEDI = mL/m2 · ELWI = mL/kg · MAP = mmHg
