
Early Protective Mechanical Ventilation is key to ARDS outcomes
The Lungsafe study demonstrated that protective ventilation is not consistently applied, reflecting the need for more accessible and effective bedside tools for identification of the lung at risk [1]. This important study concluded that ARDS is underrecognized, undertreated, and still associated with a high mortality rate.
How to prevent excess dynamic lung stress and diaphragm injury?

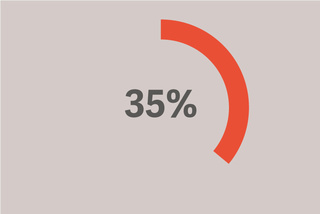
Of patients with ARDS, developed it in the first 48 hours of invasive ventilation.

Received a PEEP of less than 12.
Received a tidal volume above 8 ml/kg of PBW.
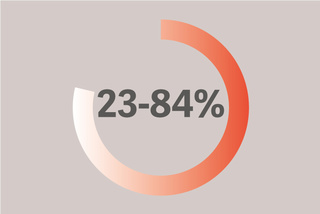
Suffers from diaphragm weakness associated with poor outcomes.
See reference [1]
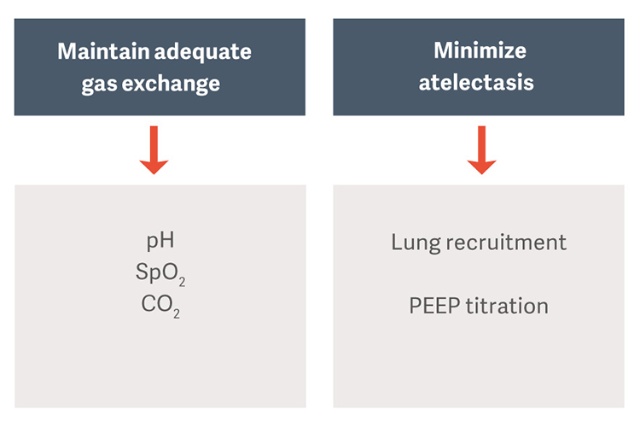
Lung and diaphragm protective ventilation
The goal of mechanical ventilation in patients with ARDS is to maintain gas exchange while avoiding the complications such as ventilator-induced lung injury (VILI), ventilator-associated pneumonia (VAP), or ventilation-induced diaphragm dysfunction (VIDD). [2]
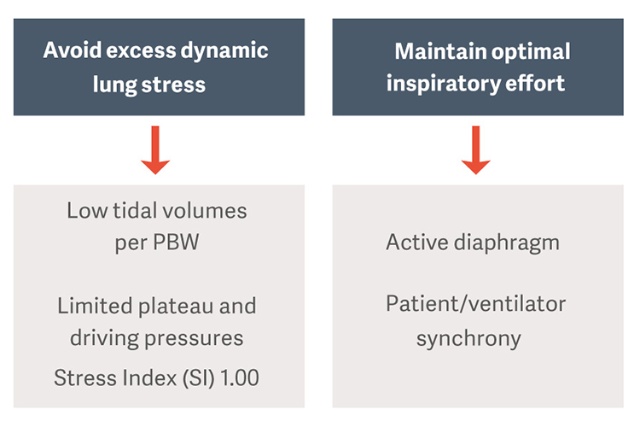
Protective ventilation strategies proposed as standard of care are prescribing low tidal volumes per predicted bodyweight (PBW), and limited plateau and driving pressures in order to reduce risk for ventilation induced lung injury (VILI) [3].
Timely recognition and prompt adherence to protective ventilation may be important for maximally reducing ICU mortality in patients with ARDS [4].
Why driving pressure?
Driving pressure (ΔP) is an indirect measurement of lung strain. It is been defined as the ratio of tidal volume by total respiratory system compliance (ΔP = VT/CRS) and can be routinely calculated for patients who are not making inspiratory efforts as the plateau pressure minus PEEP (ΔP = Pplateau - PEEP).
Amato et al identified ΔP as the main determinant of ventilator-induced lung injury (VILI), and the ventilator parameter most strongly related to mortality, particularly at ΔP values >14 cm H2O [1][3]. Targeting ΔP as means to minimize lung injury appears to be reasonable approach to improve patient outcome.
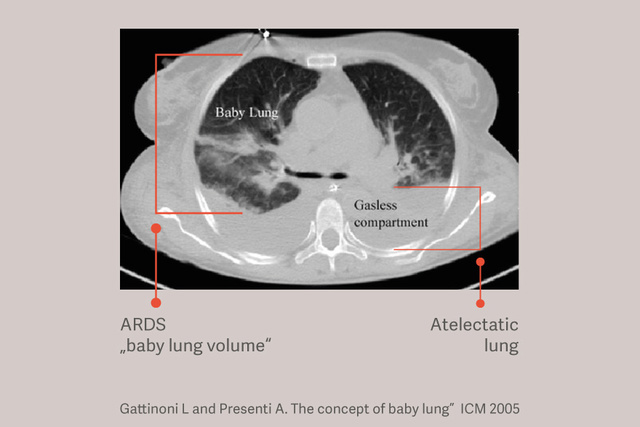
Tidal volume 6 ml/kg PBW protective
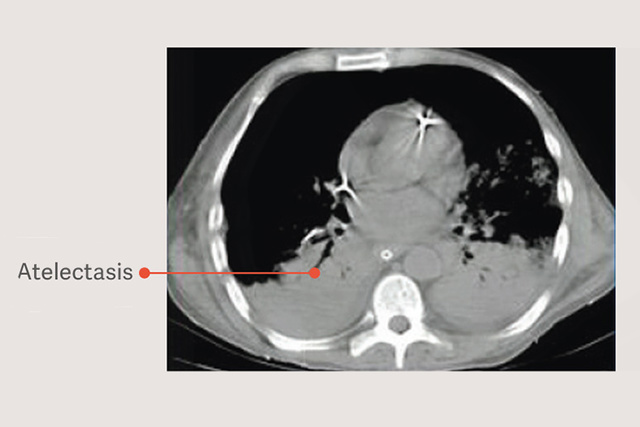
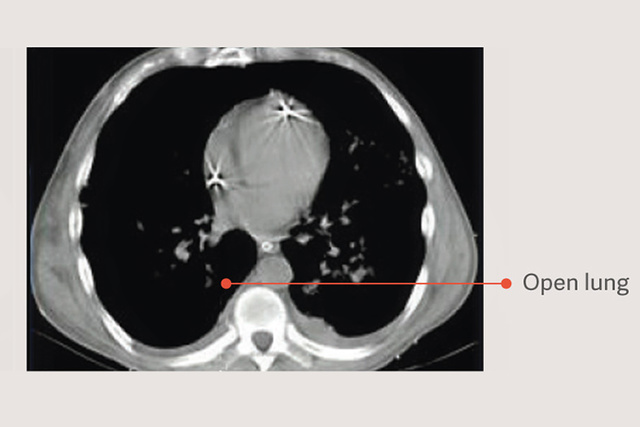
Patients with ARDS have dependent atelectasis and this atelectasis exacerbates lung injury during mechanical ventilation by reducing the size of the lung available for tidal ventilation and increasing lung stress, even when using "safe" tidal volumes.[6]
The Open Lung Approach (OLA)
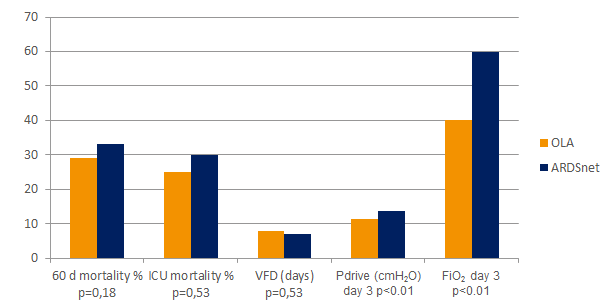
The Open Lung Approach (OLA), including lung recruitment maneuvers and PEEP titration, may dramatically improve oxygenation, while reducing lung injury.[2] [6] In the OLA trial oxygenation and driving pressure were improved, without detrimental effects on mortality, ventilator-free days or barotrauma [7]. This trial showed also one of the lowest reported mortality rates for patients with established ARDS: 25% .
Graphic reference [7]
Is there value in lung recruitment maneuvers (RM)?
Recruitment maneuvers in ventilation strategies
A recent systematic review and meta-analysis of randomized trials comparing mechanical ventilation strategies with and without RMs, showed RMs to be safe and well tolerated [8].
Maintain optimal inspiratory efforts and protect the diaphragm
Impact on clinical
The presence of diaphragm weakness significantly increases the risk of difficult weaning, prolonged weaning and hospital mortality, says Dr Ewan Goligher, referencing a recent study on the topic.[16]
