Coronary Artery Bypass
Getinge at the heart of the CABG patient

800,000 life-saving CABGs
40 years of collaborative innovation
1 shared goal: advancing patient care
Patient Satisfaction Is Integral to CABG Quality and Reimbursement
Coronary artery bypass grafting (CABG) is a common procedure, but one with significant costs and complexities. Patients often research publicly available information about hospitals and surgeons to be certain that they’re making the right choice. Patients’ shared experiences related to their CABG procedures and recovery can have important reputational and financial implications for your hospital.
The Transition from Volume-Based to Value-Based Patient Care
Healthcare systems have recognized CABG surgery as one of the most costly single surgical procedure performed in cardiac surgery. Understand how bundled-payment models and standardized care pathways may significantly impact quality improvement initiatives and positively affect the costs associated with CABG.

Improving the quality of CABG surgery
Improving CABG quality has important implications not only for clinical outcomes but for hospital reimbursement, patient satisfaction and cardiac surgeon reputation. Reducing postoperative complications is essential to meet evolving quality standards. Discover proven methods to improve outcomes for high risk CABG patients.
What drives a cardiac surgeon?
Being a cardiac surgeon is a fantastic job; it's all about saving lives and helping critically ill patients. But cardiac surgeons cannot keep hearts beating on their own; the teamwork in the OR is of greatest importance. When it comes to saving lives, we all work together as one.

Patient satisfaction is a key marker for hospital quality and performance
Studies have looked for ways to improve CABG patient outcomes. Access the white paper and understand how patient satisfaction can influence your institutional reputation.
Getinge at the heart of the CABG patient
For more than 50 years, coronary artery bypass graft (CABG) surgery has been the standard of care for revascularization of patients with coronary artery disease.[1]
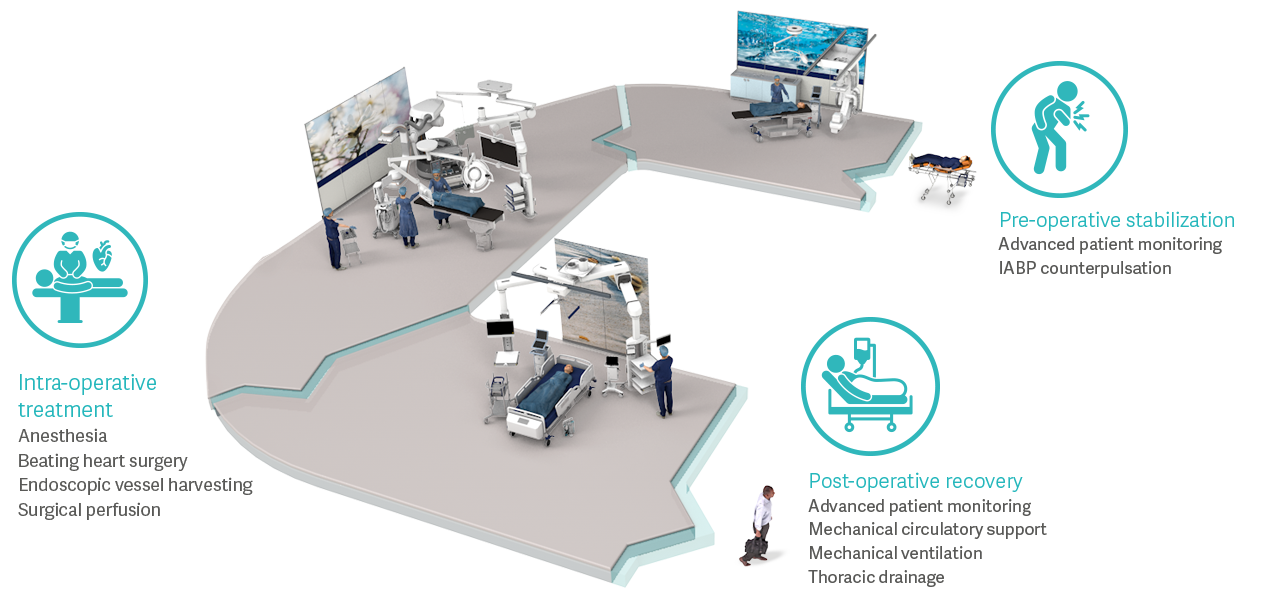
Today’s CABG patient has a higher risk profile due to multiple co-morbidities, which contributes to an increase in surgical complexity, perioperative complications and cost.[2] These patients present new challenges and have specific resource requirements, from pre-operative stabilization to intra-operative treatment and post-operative recovery.
For more than 40 years, we have shared the goal of improving your cardiac surgery service. Discover how Getinge innovations can help you enhance patient care, reduce operational costs and contribute to a positive patient experience.[3]
Pre-operative stabilization
Intra-operative treatment
Post-operative recovery
Ensuring pre-operative stabilization
More than 30% of patients presenting for CABG surgery are considered high-risk.[4] Some of these high-risk patients have predicted morbidity and mortality rates greater than 80%.[5]
Evidence-based medicine suggests that preemptive clinical protocols, which include advanced patient monitoring and a myocardial protective strategy, may help avoid procedural complications and shorten overall length of stay.[6], [7]

Advanced Patient Monitoring
Preemptive hemodynamic optimization can help avoid intra- and post-operative complications before a patient becomes critical.[6] Our tools guide you to define the best individual treatment for patients with challenging hemodynamics conditions.

IABP Counterpulsation
In the presence of ongoing ischemia or left ventricular dysfunction, pre-operative IABP counterpulsation therapy can provide myocardial protection by reducing perioperative myocardial ischemia, stabilizing hemodynamics and improving coronary perfusion.[7]
The benefits of pre-operative IABP counterpulsation for high risk CABG patients
In this webinar, Dr. Joseph L. Thomas presents his expert opinion, the physiologic basis for pre-operative IABP counterpulsation and the existing clinical data in support of this treatment strategy.
Enabling intra-operative treatment
Approximately 33% of patients experience at least one complication following CABG surgery, of which nearly 40% of these patients suffer one or more major morbidities.[2]
Today’s high-risk patient requires innovative therapies and devices to minimize the risk of post-op complications. Whether it is the delivery of anesthesia, beating heart surgery or supporting a failing heart, using the right tool can help reduce complications, ventilation time and hospital costs.

Anesthesia
Anesthesia is a standard part of intra-operative care. When combined with advanced ventilation strategies, it can help reduce postoperative complications, minimize agent usage, and give you more time to focus on patients.[8]

Endoscopic Vessel Harvesting
Endoscopic vessel harvesting (EVH) is at the forefront of technological advances that improve vessel harvesting for coronary artery bypass graft (CABG) surgery. The EVH procedure uses a smaller incision to obtain a bypass conduit for CABG than traditional vessel harvesting procedures, leading to faster recovery, better clinical outcomes, and enhanced patient satisfaction.

Surgical Perfusion
Perfusion systems are a standard part of intra-operative care. Our devices have been used successfully for millions of cardiopulmonary bypass procedures worldwide.
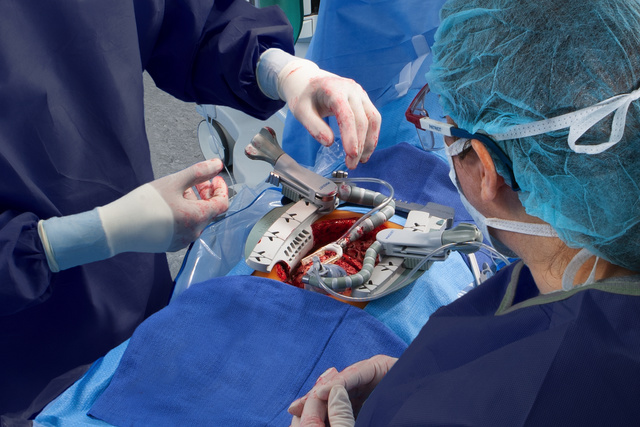
Beating Heart Surgery
Off-pump coronary artery bypass (OPCAB) reduces patient morbidity and mortality, decreases the incidence of acute renal failure, reduces transfusions, improves post-surgery neurological outcomes, decreases postoperative stroke risk, and shortens recovery times as an alternative to on-pump surgery.
Supporting post-operative recovery
Low cardiac output syndrome and prolonged mechanical ventilation are common and costly post-operative complications following CABG surgery.[2], [10]
Fortunately, there are advanced technologies that can facilitate successful management of these complications. Using the right tool can help patients recover faster through goal-directed therapy with the advanced patient monitoring systems, a variety of mechanical circulatory support devices, or protective ventilation strategies.

Advanced Patient Monitoring
Avoid intra- and post-operative complications with perioperative hemodynamic optimization — before a patient becomes critical. Our tools guide you to define the best individual treatment for patients with challenging hemodynamics conditions.[6]

Mechanical Circulatory Support
Ensure personalized support for patients with hemodynamic instability. Our solutions offer the option to deliver partial to full level support of the heart and/or lungs.

Mechanical Ventilation

Thoracic Drainage
Getinge offers a full line of thoracic drainage products, as well as a line of mobile drains to facilitate early ambulation. With decades of experience as the leader in thoracic drainage products, Getinge sets the bar for clinical performance.
Getinge solutions along the clinical pathway
In everything that we do, we consider the complexity of hospitals‘ needs, and the value of over-arching support along the complete in-hospital clinical pathway.
Our products for CABG surgery serve crucial steps along the pathway of treatment and recovery, particularly for your highest-risk patients. Our solutions make us the preferred Medtech partner to help improve efficiency and outcomes for CABG procedures.