Less sedated ICU patient during mechanical ventilation
Dr Torben Steensgard Anderssen - Senior consultant ICU at Vejle Hospital explain through those two videos the benefits of the low sedation ventilation strategy.
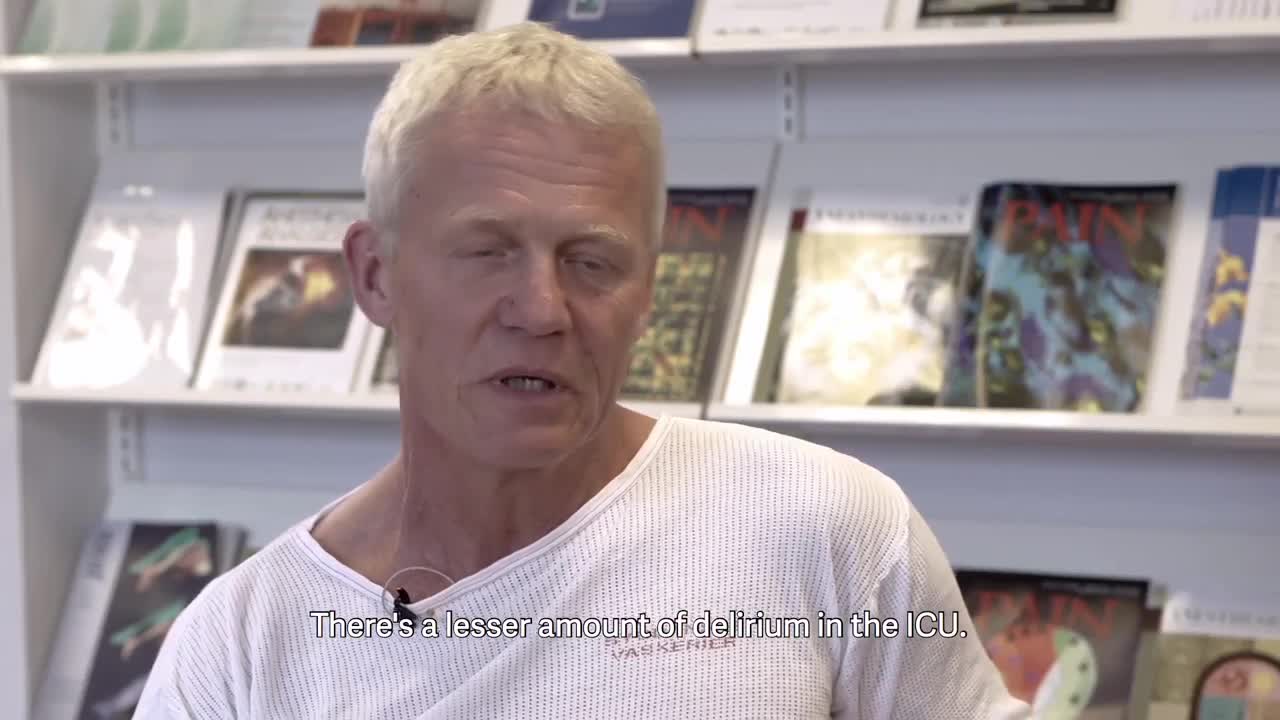
He explains that the key to having less sedated and actively participating patients is to be able to meet their breathing needs. To try and sustain their natural breathing effort as much as possible.
The clinical experience of less sedation and more awake patients
Dr Andersen is able to communicate with his patients at almost any time. Watch the video and learn more about his work and what challenges he faced when lowering the sedation. From the science behind the decision to their clinical experience today.
"We are able to communicate with our patients at almost any time", says Dr Andersen
The key to having less sedated and actively participating patients is to be able to meet their breathing needs. To try and sustain their natural breathing effort as much as possible.
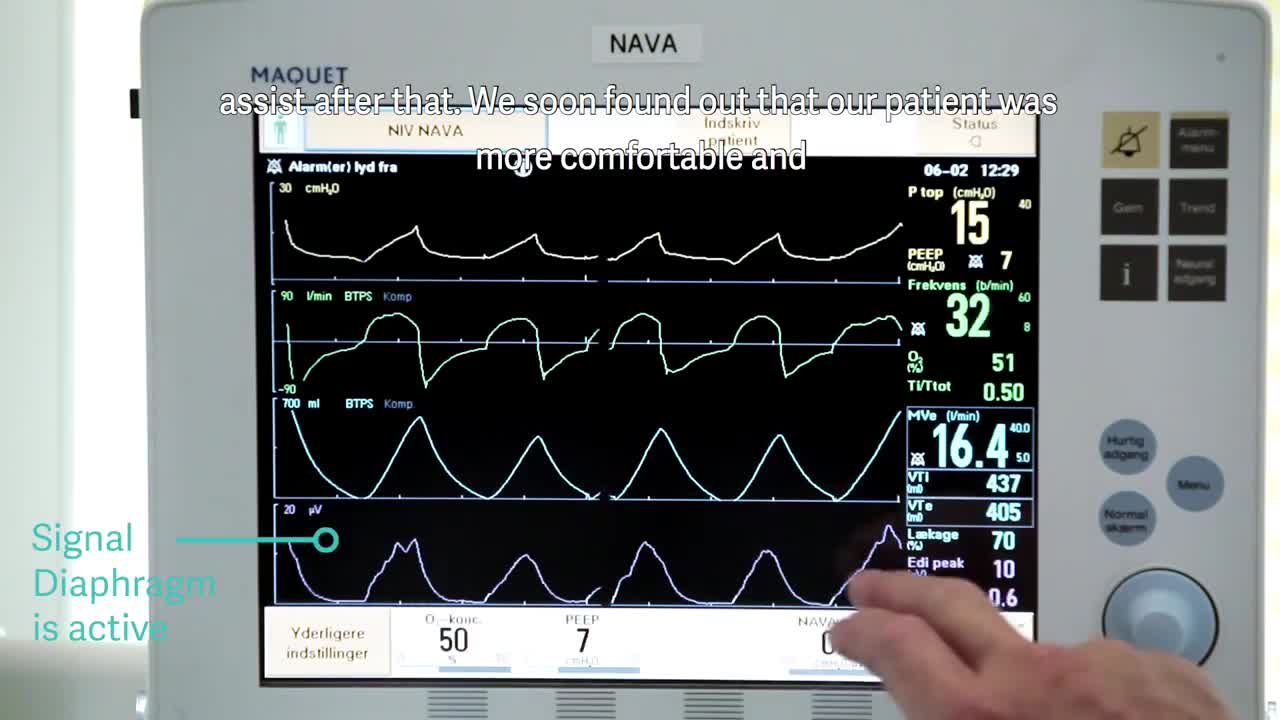
This is when monitoring the electrical activity of the diaphragm (Edi), has become especially useful for Dr. Andersen. It has helped him identify patient-ventilator asynchrony and reduce over-sedation and over-assist.