Mechanical ventilation
With people in mind
Our goal is to help keep your adult, pediatric and neonatal patients as safe and comfortable as possible with easy to use, easy to apply ventilation.
Why you will love to work with a Servo Ventilator
Increase patient safety
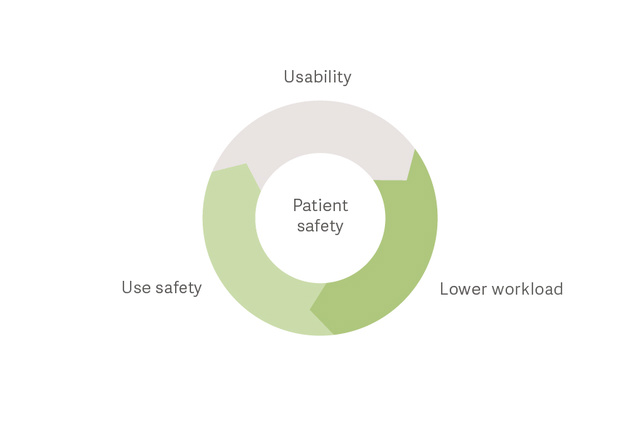
Reduce workload and limit use errors and close calls with a Servo Ventilator.[1]
Adapt to your needs
Provide quality ventilation for every situation and for patients of all sizes, from neonates through adults.
Secure your investment
Reliable performance, low maintenance and easy connection to your hospital systems.
Increase patient safety
Keep your patients safer and reduce staff workload
A recent study in Critical Care showed that by choosing an easy-to-use mechanical ventilator you can positively impact patient safety and staff workload.[1]

The Servo Ventilator story
This is a story of a revolution. One that would change our perception of intensive care ventilation forever. A scientific wonder that captivated the medical world more than fifty years ago, and one that pioneered our understanding of personalized ventilation we know today. We called it the Servo ventilator. The world’s first flow-controlled ventilator with a rapid servo control system.
Deliver optimal ventilation and wean earlier

Challenge: Avoid intubation in patients with respiratory failure
Non-invasive respiratory support can reduce the need for intubation and resulting complications such as ventilator-associated pneumonia (VAP),[7] excessive sedation,[8] delirium [9] and ICU-acquired weakness.[10] Non-invasive support allows patients to remain active, a strategy now adopted in many ICUs. Servo-u offers multiple options to support your patients with non-invasive therapies.

Challenge: Prevent ventilator-induced lung injury (VILI) during assisted ventilation
Studies have demonstrated that Neurally Adjusted Ventilatory Assist (NAVA) promotes lung protective spontaneous breathing with improved patient-ventilator synchrony and gas exchange.[14] [15] While on NAVA, the respiratory centers and reflexes in the lungs and upper airways will instantly limit tidal volumes when the lungs are overdistended. This gives patients the opportunity to choose their own tidal volumes and respiratory patterns, which may limit VILI.[16] [17]
Challenge: Prevent delayed weaning
A recent study shows that 29% of patients experience weaning failure due to diaphragm dysfunction. It extends time on mechanical ventilation by up to 16 days.[18] But thanks to NAVA ventilation you can have a more comfortable patient with less sedation and an active diaphragm, which may help you promote early weaning.[2] [3] [4] Furthermore, monitoring diaphragm activity (Edi) can help you assess weaning readiness and monitor work of breathing during recovery, even when there is no ventilator support.[27]

Secure your investment and take the stress out of ownership

Cost-effective care
Servo Ventilators are easy to learn and use, have few parts to clean, and are easy to maintain, which promotes minimal training time and high staff efficiency.
Connected to your environment
Servo Ventilators connect to a number of PDMS systems and patient monitors.[1] An HL7 converter makes the system conform to IHE technical framework.
Smart fleet management
Similar look and feel between ventilators and interchangeable plug-in modules increase convenience and allows for high acuity ventilators to work alongside more mobile solutions.
Explore our products
Find the right products and solutions for you
