Ethics and sustainability
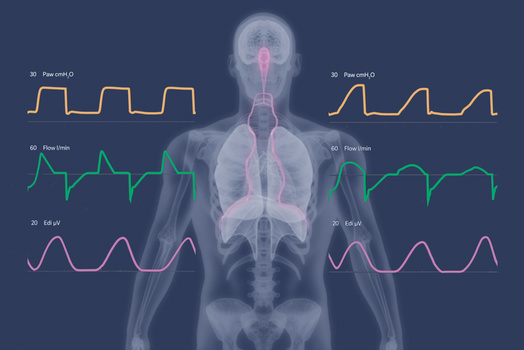
Getinge’s sustainability work is an integral part of our passion for life. We help our customers save lives with a commitment to conducting business that is socially, ethically and environmentally sound across the entire value chain.

Investors - making a difference
We believe in making a difference. And our heritage proves that passion for improving patient outcome, through leading technology and integrated medtech solutions, adds value to both healthcare and investors.
Latest news & updates
View allEvents
All eventsHow can we help? Please contact us
Come work with us
A career at Getinge offers a dynamic, international environment with a market leading company. Find out more about working here and where you can make a difference.