Personalized ventilation for better outcomes
As our most advanced ventilator, Servo-u builds on more than 50 years of groundbreaking innovations. It features unique decision support tools such as Transpulmonary pressure, Open Lung Tool, Servo Compass®, Stress Index, and Edi – the electrical activity of the diaphragm. Crucially, it also comes with our unique NAVA ventilation mode. In other words, an all-in-one solution where there’s no need to switch ventilators or devices.
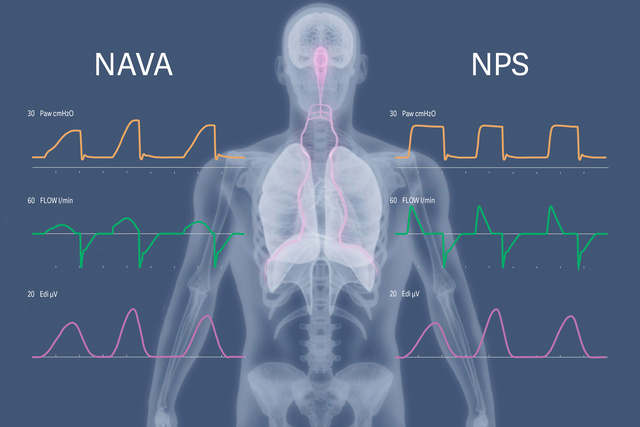
Neural Pressure Support (NPS) and NIV NPS
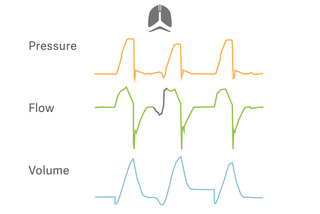
NPS and NIV NPS is a complement to NAVA and NIV NAVA, delivering time-synchronized pressure support (PS), where both breath triggering and flow termination are based on the patient’s neural respiratory drive. NPS may help reduce the incidence of premature expiratory cycling and harmful eccentric diaphragm contractions, which are common with conventional flow-cycled PS. The faster pressurization rate compared to NAVA may offer advantages in managing restrictive ARDS and obstructive COPD patients.

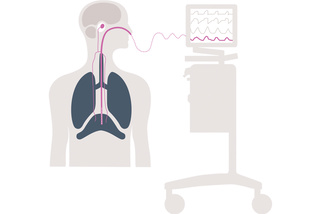
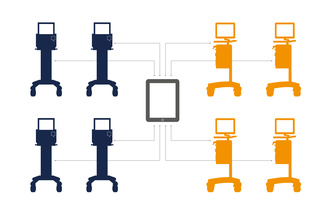
Servo TwinView - a virtual twin of Servo-u ventilator
Servo TwinView provides remote near real-time data from your Servo-u and Servo-n ventilators. Irrespective on where you access Servo TwinView, the information is presented in the same way as on the ventilator.
- More effective rounding and handover
- Remote second opinions and support
- Support for onboarding and training
- Reduced patient disturbance


Personalized lung protection
Servo-u offers you the complete toolkit for personalized ventilation. It enables you to detect risks early and support timely and consistent implementation of personalized protective ventilation strategies, in line with the latest international guidelines.[2],[3] In other words, the right support for each patient, at the right time.

Personalized weaning
Recent clinical studies reveal that diaphragm weakness is prevalent (23–84%) in ICU patients and consistently associated with poor outcome.[4] Servo-u lets you monitor the patient‘s diaphragm activity (Edi) to personalize ventilation for successful weaning. A recent study showed NAVA shortens time of mechanical ventilation by almost 35%.[5]

Secure and sustainable
Servo-u is a secure solution that was developed with efficiency and sustainability in mind – fewer parts, long-lasting materials that are easy to reprocess and sourced responsibly. Several components are interchangeable with other Servo ventilators, to help optimize uptime and reduce purchase and maintenance costs. And with many service centers globally, we are always there to support your hospital.

Whether it’s a 300-gram newborn or a larger adult, every patient has special needs. Which is why we offer personalized ventilation to help tailor your treatments. Servo-u is our most complete ventilator, offering a wide range of tools and therapies for advanced care.
Produkty powiązane

Context-based guidance
Servo-u provides informative guidance for everything from pre-use check to initial parameter setting and throughout the entire treatment.

Safety Scale parameters
The system Safety Scale tool makes parameter changes quick and intuitive, while dynamic images illustrate how those changes may affect ventilation.

Choose your view
- Basic, Advanced and Loops
- Distance and Family
- Servo Compass and Pes & PL

Alarm management
The frame lights up when an alarm is triggered, and this visual signal is easy to see from any view point. On-screen checklists help you to manage each active alarm and avoid undesired alarms.
Protect the lungs and other organs
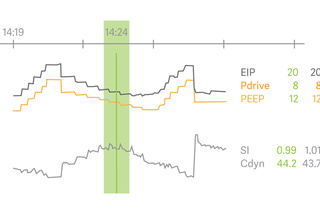
Servo Compass
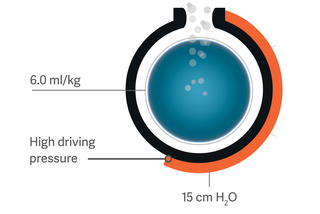
Servo Compass makes it easy to see when plateau/driving pressure or tidal volume per predicted body weight (VT/PBW) are off pre-defined targets and interventions are needed.[6] Precisely calculated Dynamic compliance (Cdyn) and Stress index (SI) complete the picture, helping you detect changes in lung volume and verify over-distension. [7],[8],[9]

Transpulmonary pressure
To simplify esophageal manometry and improve accuracy, we have developed an automatic maneuver to validate balloon positioning and filling. A diagnostic view provides esophageal (Pes) and transpulmonary (PL) pressure waveforms, with key parameters for safety assessment of controlled and spontaneous ventilation. The relationship between airway and transpulmonary pressures is now much more intuitive.
Open Lung Tool
Open Lung Tool trends helps you assess lung mechanics and gas exchange – breath-by-breath, in real time and retrospectively. It provides flexibility and guidance when personalizing PEEP and driving pressure during recruitment maneuvers, prone positioning and extracorporeal life support. Stress index, carbon dioxide elimination and transpulmonary pressures are also fully integrated.
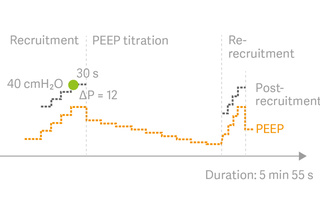
Automatic recruitment maneuvers
Auto SRM is an automatic workflow for Stepwise recruitment maneuvers based on the Open Lung approach.[10]
The tool guides you smoothly through recruitment, decremental PEEP titration, re-recruitment and post-recruitment personalization of PEEP and driving pressure, based on optimal Cdyn. Diagnostic features include assessment of recruitability and additional decision support when patients do not respond to the recruitment maneuver.[11]
Wean early with an active diaphragm
Target protective tidal volumes
PRVC is a true volume-targeted mode that automatically adapts the inspiratory pressure to account for rapid changes in lung mechanics. Separated regulation
of controlled and assisted breaths reduces tidal volume variations and ensures lower driving pressure. A low tidal volume strategy can therefore be maintained
when a patients start breathing spontaneously.

Ease the transition to spontaneous breathing
The interactive Automode eases the transition to spontaneous breathing for patients and staff. It switches seamlessly between controlled and supported modes depending on patient effort. There are three combinations available for Automode:
- PC ⇆ PS
- PRVC ⇆ VS
- VC ⇆ VS
Diagnose breathing and start weaning
Edi – the vital sign of respiration – is a bedside diagnostic tool that allows you to monitor and safeguard the patients diaphragm activity.[12],[13] Servo-u lets you visualize Edi on screen, making it easier to identify over-assist, over-sedation and asynchrony when optimizing ventilation delivery and assessing weaning readiness. The result: earlier and more informed interventions.[6],[10]

Activate the diaphragm and protect the lungs
NAVA (Neurally Adjusted Ventilatory Assist) uses the Edi to deliver personalized support, invasively and noninvasively. It promotes lung protective spontaneous breathing with higher diaphragmatic efficiency, and fewer periods of over and under-assist.[14],[15],[16],[17],[18],[19],[20] It also improves the patient’s ICU experience, helping you to reduce sedation with improved comfort and sleep quality.[5],[21],[22],[23],[24],[25]

High-flow therapy
High-flow therapy that reduces the patient’s work of breathing through an accurate flow of heated and humidified oxygen, improving comfort and tolerance.[31] There is no need to switch to a separate high-flow system, and the workflow supports both delivery through non-invasive, and invasive tracheostomy interfaces.
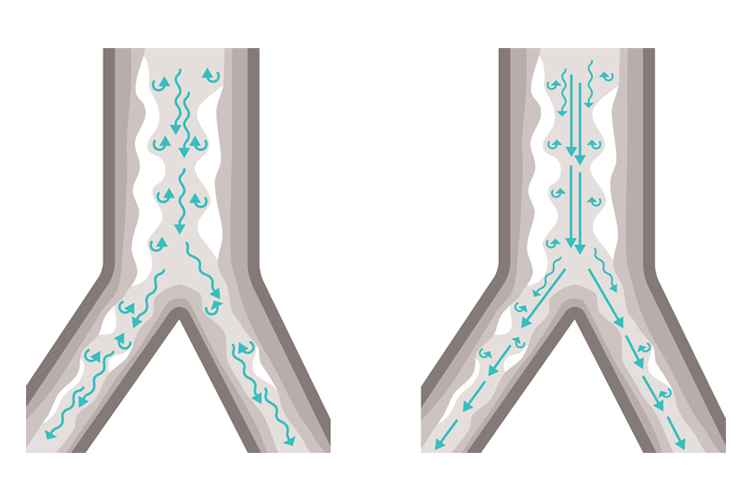
Soothing Heliox therapy
Heliox is our therapy option for patients having difficulty breathing due to airway resistance associated with various types of respiratory disease. Safe, reliable and easy to use, Heliox is a mixture of helium and oxygen that, due to its low density, facilitates laminar flow and minimizes airway pressure. The illustration above shows Heliox therapy promotes better laminar flow with less turbulence in a typical asthma patient.[32]

Improve comfort with integrated Aerogen® nebulizer
Aerogen® nebulizer – this fully integrated feature offers a significantly higher lung deposition compared to jet nebulizers.[33] Its closed-circuit medication filling design mitigates transmission of patient-generated infectious aerosols.[34] For the recovering patient, Edi real-time respiratory drive monitoring will precisely quantify the effect of the above therapies.[35],[36]

A modular platform
A range of software options and inter-changeable hardware modules allows you to configure to your current needs and upgrade as those needs change. It also means modules can be moved between ventilators, lowering overall costs.

High quality consumables
We offer an extensive range of readily available consumables designed with patient safety and ease of use in mind - all to help secure your everyday operations.
Connected to your data
Talis helps you to connect your Servo fleet to your HIS or patient data management system (PDMS). Data is transferred in real time to support clinical decision-making.

Maximum uptime
Optimizing your equipment’s services is often an untapped opportunity to maximize productivity and reduce costs. Our Getinge Care service offering allows you to focus on what’s important - saving lives.
Simple to learn, safer to use
Simple to learn, safer to use
An alarm light indicator around the upper frame
of the screen is visible from all directions.
Alarms are shown in three colors: red (highest
priority), yellow (medium priority), and blue (low
priority). Alarm indication is shown in two ways:
blinking value (measured or indicated) and
alarm message in the alarm message area.
You can save up to 40 screen shots or recordings on the
ventilator. Or export them to a USB drive. To make a screen
shot, press the Camera button or, to record waveform data,
press the video recorder button. Trends and data can be
saved by pressing the Media button and saved in the
trends and logs library for later viewing.
If you need additional values, press this green arrow
and you’ll get all the parameters that are measured in
ventilation mode you are using. And when you press the
Mode arrow, you can see all the set parameters.
A post-recruitment summary with color-coded results
and personalized settings provides further clinical
decision-support.
The additional settings button lets you quickly access
other ventilatory modes or therapies, as needed.
You can also quickly return to the main settings at any
time by pressing here.
The screen can be rotated through 360°, which means
you can place the ventilator anywhere around the bed
depending on clinical requirements
Intuitive touchscreen
The intuitive touchscreen makes Servo-u a breeze to learn and use. Information texts, dynamic images and workflow support help staff to orientate quickly and follow guidelines. The interface also simplify knowledge sharing with the intuitive touchscreen, making it easy to retrieve screenshots and recordings or connect to a larger screen.
Flexibility through ergonomic design
Servo-u features an ergonomic design. The screen can be rotated through 360°, which means you can place the ventilator anywhere around the bed, depending on clinical requirements. You can also mount Servo-u on a ceiling supply unit or shelf. The system is light and compact, making it highly suitable for intra-hospital transport.
Personalized lung protection, breath by breath
Recent clinical studies suggest that many ventilators lack effective bedside decision-support tools. It's a problem that results in protective ventilation strategies being delayed or inconsistently applied. Ultimately, this can harm the patient and worsen the outcome.[2],[7],[37] To avoid these situations, Servo-u offers you the complete toolkit for personalized ventilation.

Personalized weaning with lung- and diaphragm-protective ventilation
Respiratory drive and effort monitored by electrical activity of the diaphragm (Edi) or esophageal pressure (Pes). Weaning support through Automode, NAVA, High Flow and Heliox therapy
NAVA shortens time of mechanical ventilation by almost 35%.[5]

Target protective volumes and pressures
PRVC is a true volume-targeted mode that automatically adapts the inspiratory pressure to account for rapid changes in lung mechanics. Separated regulation of controlled and assisted breaths reduces tidal volume variations and ensures lower driving pressure. A low tidal volume strategy can therefore be maintained when a patient start breathing spontaneously.
Our interactive Automode eases the transition to spontaneous breathing for patients and staff. It switches seamlessly between controlled and supported modes, depending on patient effort.

Diagnose breathing to facilitate weaning
Edi – the vital sign of respiration – is a bedside diagnostic tool that allows you to monitor respiratory drive and effort and safeguard the patients diaphragm activity.[12],[13] With the Edi signal continuously visible, you can detect diaphragm inactivity, over-sedation, patient ventilator asynchrony as well as over- and under-assist. You can also monitor changes in increased work-of-breathing during weaning trials and post-extubation. Edi monitoring is available in all invasive and non-invasive ventilation modes, and can be used from day zero to discharge from the intensive care unit.

Exercise the diaphragm and protect the lungs
NAVA (Neurally Adjusted Ventilatory Assist) follows the patient’s Edi to personalize lung-protective spontaneous breathing with higher diaphragmatic efficiency, and fewer periods of over and under-assist. NAVA shortens the time of weaning and mechanical ventilation and increases the number of ventilator-free days. NIV NAVA significantly improves patient-ventilator interaction, and reduces NIV complications.[38] For patients with acute exacerbation of COPD it can be effective in managing their status and to improve patient outcomes.[27],[38],[39],[40],[41]

Improve comfort with effective therapies
High Flow therapy reduces the patient’s work-of-breathing by providing an accurate flow of humidified gas with a set oxygen concentration.
Heliox therapy is designed for patients with airway resistance diseases.
Aerogen® nebulizer – this fully integrated feature offers a significantly higher lung deposition compared to jet nebulizers. Its closed-circuit medication filling design mitigates transmission of patient-generated infectious aerosols. For the recovering patient, Edi real-time respiratory drive monitoring will precisely quantify the effect of the above therapies

A sustainable solution based on efficiency and responsibility
Servo-u is a sustainable solution on multiple levels: Fewer parts that are long-lasting and easy to reprocess sourced responsibly, interchangeable with other Servos and always supporting your uptime. A flexible, modular platform that can be easily upgraded for your evolving clinical needs. Expert support at hand if needed. In other words, less waste, more productivity and a better environment for all.
For me, this is a secure investment – a solid product to build on, based on a solid foundation.
Intensive care physician and researcher, Brazil
Sustainability through efficiency
The Servo-u adds efficiency, drives down maintenance costs and
reduces waste. It shares many components and parts with other Servo
ventilators. Hot swappable batteries, for example, and easy- to-clean
expiratory cassettes that are interchangeable, meaning you can use
any cassette that is ready for use if a patient is waiting. You can also
choose from a range of consumables such as catheters, nebulizers and
interfaces. All original parts and consumables are optimized for lasting
high performance.
Extra support with Getinge Care
With many service centers globally, we are always close at hand. To
maximize uptime, ask us about local service agreements. Our Getinge
Care package, for example, comes in four different levels of support
depending on your needs. Whatever your specific situation, our skilled
service technicians and staff, many of whom are clinicians, are always
there to support you. Servo-u is also designed for a high degree
of connectivity: the ventilator connects to a wide range of PDMS
systems and patient monitors. It can also use MSync (optional) as
an HL7 converter, which makes the system conform to IHE Technical
Frameworks
Marketing Sales - Brochures
-
Servo-u gives you many options for personalized lung protection and weaning, for treatment of all patient categories. All are easy to understand, implement and use.
-
The physiological challenges of mechanical ventilation requires a powerful toolkit, offering the right protection for each patient at the right time.
-
Achieve faster personalized weaning with lung and diaphragm-protective ventilation.
-
Help patients suffering from obstructive lung diseases, such as asthma, bronchiolitis, and COPD, breathe easier where additional targeted support may be required.
Marketing Sales - Sales Flyer
-
Expand the performance of your flexible Servo-u with additional functionalities and features allowing you to adapt more easily to your ever-changing clinical needs.
Marketing Sales - Data Sheet
-
Detect electrical activity of diaphragm, with our range of Edi catheters, enabling NAVA and NIV NAVA ventilation modes, and available in all patient categories.
-
The NutriVent is a nasogastric feeding tube with one or two balloons for monitoring of esophageal, transpulmonary and gastric pressures.
Marketing Sales - Other
-
Official product environmental profile for the Getinge Servo-u ventilator system
Visit our Academy – training and education designed to enhance your proficiency
For more information about our onsite events or remote trainings, you can also contact your local sales & service representative.



